Depression

Definition and Incidence of Depression:
Also Major or Clinical Depression is a common and serious mood disorder. It causes severe symptoms that affect how you feel, think, and handle daily activities, such as sleeping, eating, or working. The symptoms must represent a change from previous functioning and be present for at least two weeks to meet criteria for a diagnosis. Depression in more common in women to men 8.7% vs. 5.3%. It is frequently recurrent in more severe cases and requires ongoing treatment in these patients.
Signs and Symptoms of Depression:
Must be persistent and present for at least two weeks: 1. Sad, empty or anxious mood 2. Feelings of hopelessness, helplessness 3. Thoughts of death or suicide, or suicide attempts 4. Loss of interest or pleasure in hobbies and activities 5. Feelings of guilt or worthlessness 6. Decreased energy or fatigue 7. Moving or talking more slowly 8. Difficulty concentrating, remembering, or making decisions 9. Difficulty sleeping, early-morning awakening, or oversleeping 10. Appetite and/or weight changes 11. Aches or pains, headaches, cramps, or digestive problems without a clear physical cause and/or that do not ease even with treatment 12. Feeling restless, having trouble sitting still or irritable
Other Types of Depression:
1. Dysthymia: A depressed mood that is less severe and lasts for at least two years. 2. Postpartum Depression: Women that experience major depression during pregnancy or after delivery, more serious than the common “baby blues”. The feelings of extreme sadness, anxiety, and exhaustion may make it difficult to complete daily routines and care activities for their family. 3. Seasonal Affective Disorder: Depression that starts during the winter months, when there is less natural sunlight. This depression generally lifts during spring and summer. 4. Psychotic Depression: A more severe type of depression with symptoms of psychosis, such as paranoia, delusions of guilt, somatic delusions, visions and hallucinations. Usually a more severe type of depression, which may overlap with schizophrenia, bipolar disorder, alcoholism, dementia and other organic brain disease. 5. Depression in Bipolar Disorder: Bipolar disorder may cause episodes of extremely low moods, but may switch to mixed state with increased agitation and suicidal thoughts, or uncontrolled mood elevation hypo-mania and mania. Treatment of bipolar disorder usually requires mood stabilizers and antipsychoics 6. Depression in Personality Disorders: Personality disorders are often coexisting with depression and contribute to depression symptoms. Treatment of underlying personality disorders is usually by psychotherapy or CBT.
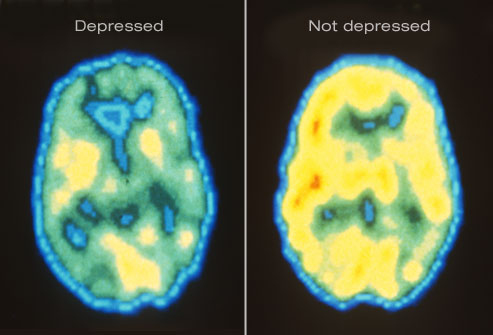
Shown here are PET scans of the brain showing different activity levels in a person with depression, compared to a person without depression.
Causes of Depression:
1. Genetic: research shows depression can run in families. Studies of twins show a 40-50% chance of the other being affected. 2. Traumatic Childhood: 10-30% chance depending if one or both parents are depressed. 3. Personality Style: Dependent Personality, Anxious Personality, Perfectionism, or Schizoid Personality are not helpful. 4. Life Events: Such as death of immediate family, financial disaster, illness and chronic pain. 5. Biologic Factors: Hormonal changes, PMS, Post-Partum depression, Menopause, seasonal changes, shift work, international travel, old age. 6. Psychiatric Illness Co-Morbidity: Other psychiatric illness such as Anxiety Disorders, ADHD, Schizophrenia, Bipolar Disorder, Dementia, Alcohol and Substance Use. 7. Medical Illness Co-Morbidity: Many severe medical illnesses are linked with increased depression, including diabetes, cardio-vascular disease, auto-immune disorders, chronic pain…see also: Depression and Medical Illness NIMH
Treatment of Depression:
Untreated depression is a costly illness in terms of decreased productivity, people feel unable to work or perform their usual household activities including caring for dependent children. Untreated severe depression may result in suicide, treatment resistance and development of chronic symptoms.
1. Medications: called antidepressants work very well in 33% of patients, fairly well in another 33%, and the remainder have poor response. They can take 1 to 2 weeks to work. Antidepressants can have variable side effects, some patients have none. The selection of antidepressant medications is complex and adequate dose and time of treatment is important in the process of recovery and effective relapse prevention. Anti-depressants available today – SSRI’s such as Prozac (fluoxetine), Paxil (paroxetine), Celexa (citalopram), and Zoloft (sertraline); Tri-cyclic antidepressants such as Elavil (amitryptiline), Sinequan (doxepin), and Tofranil (imipramine); MAOI’s such as Nardil (phenelzine); and anti-depressants with unique mechanisms of action such as Effexor (venlafaxine), Wellbutrin (buproprion) and Serzone (nefazodone).
2. Psychotherapy: helps by teaching new ways of thinking and behaving, and changing habits that may be contributing to depression. Therapy can help you understand and work through difficult relationships or situations that may be causing your depression or making it worse.
3. Electroconvulsive therapy (ECT) and other brain stimulation therapies may be an option for people with severe depression who do not respond to antidepressant medications. ECT, RTMS, MST 2011.06
4. Treatment Resistant Depression: Augmentation: There are many augmentation strategies, most useful are adding Atypical Antipsychotics, Lithium, Lamotrigen, Omega-3 Fish oil, NAC, MFolate: TRD AAPs Augmentation 2005, Augmentation and Adjunct Rx 2011.06
Helpful information for Patients:
3. Depression and Medical Illness NIMH
6. Depression Infographic Knowing Neurons 2013