Marijuana, Alcohol, SUD and Mental Health
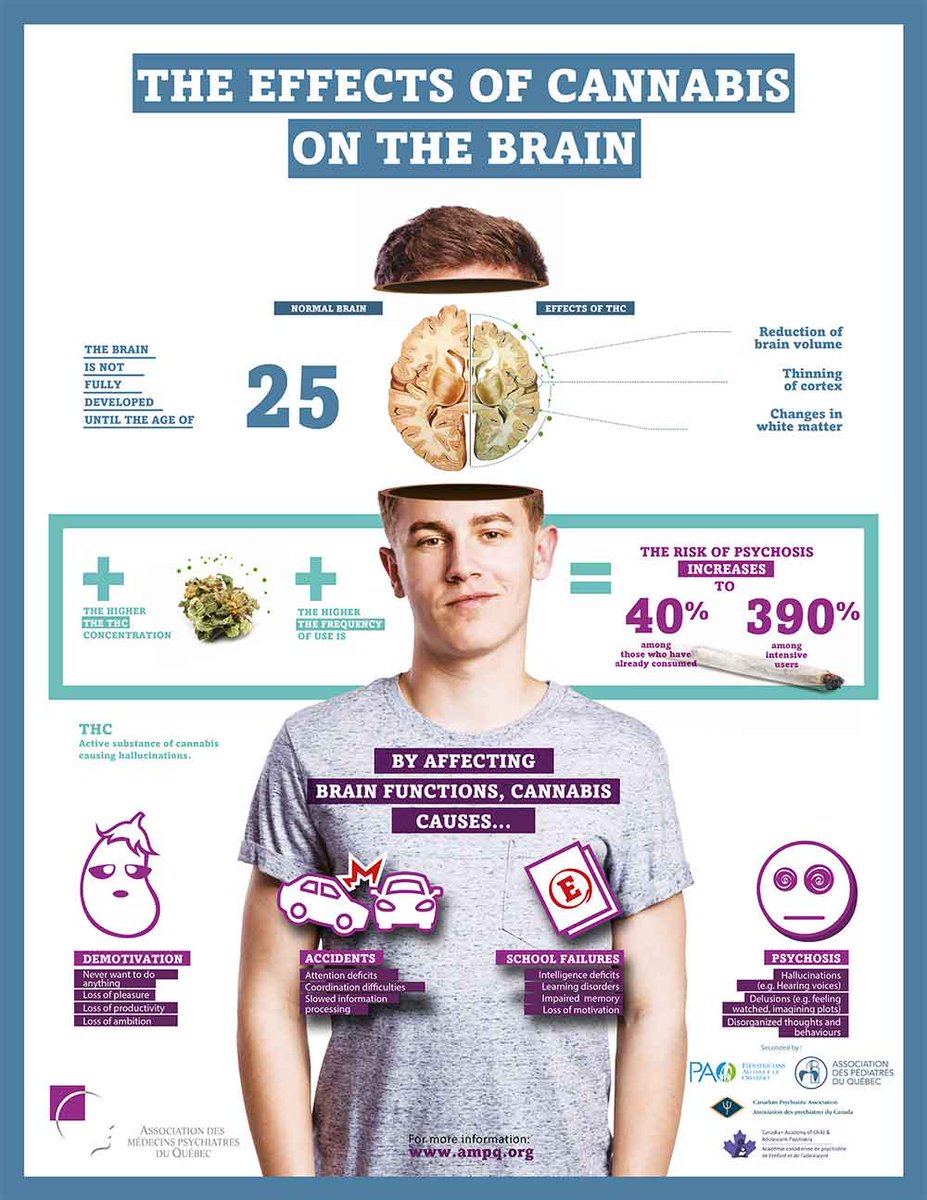
Marijuana Effect on Brain Function: Marijuana remains a controversial drug that consists of complex mixture of psychoactive substances that affects brain function. Recent reports show that fewer adolescents believe that regular cannabis use is harmful to health. Concomitantly, adolescents are initiating cannabis use at younger ages, and more adolescents are using cannabis on a daily basis. In adolescents, one of the main concerns is THC’s ability to bind easily to one receptor, called CB1. These receptors are found all over the brain, but they are particularly common in areas associated with reward and executive functioning — which includes memory and decision-making. CB1 is more abundant in adolescent brains than in adult ones.
2012 Meier Study: Meier and her colleagues analyzed the effect of cannabis use into adulthood. The study was to test the association between persistent cannabis use and neuropsychological decline and determine whether decline is concentrated among adolescent-onset cannabis users. Participants were members of the Dunedin Study, a prospective study of a birth cohort of 1,037 individuals followed from birth (1972/1973) to age 38 y. Cannabis use was ascertained in interviews at ages 18, 21, 26, 32, and 38 y. Neuropsychological testing was conducted at age 13 y, before initiation of cannabis use, and again at age 38 y, after a pattern of persistent cannabis use had developed. Persistent cannabis use was associated with neuropsychological decline broadly across domains of functioning, even after control- ling for years of education. Informants also reported noticing more cognitive problems for persistent cannabis users. Impairment was concentrated among adolescent-onset cannabis users, with more persistent use associated with greater decline. Further, cessation of cannabis use did not fully restore neuropsychological functioning among adolescent onset cannabis users. Findings are suggestive of a neurotoxic effect of cannabis on the adolescent brain and highlight the importance of prevention and policy efforts targeting adolescents.
In adolescents, one of the main concerns is THC’s ability to bind easily to one receptor, called CB1. These receptors are found all over the brain, but they are particularly common in areas associated with reward and executive functioning — which includes memory and decision-making. CB1 is more abundant in adolescent brains than in adult ones.
Ref: meier-et-al-2012-persistent-cannabis-users-show-neuropsychological-decline-from-childhood-to-midlife
Marijuana Legalisation: Despite these concerns the Canadian Government supports the commercialization of medical and recreational marijuana, resulting in significant increase in marijuana usage across the population including teens. The question is: was the liberalization of medical cannabis and the legalization of nonmedical cannabis in Canada associated with changes in the population-attributable fraction of
cannabis use disorders associated with schizophrenia?
Findings In this Ontario population-based cohort study comprising 13 588 681 individuals, the population-attributable fraction of cannabis use disorder associated with schizophrenia increased significantly from 3.7% in the prelegalization period to 10.3% during the postlegalization period. Meaning These findings suggest that the association between cannabis use disorders and schizophrenia is an important consideration for the legalization of cannabis.
Ref: Psychosis incidence after Marijuana legalisation
Concurrent Disorders: Cognitive changes with SUD (Substance Use Disorder): A broader clinical issue is in people with substance use disorders there is well known cognitive decline, that can be found during both the dependence and drug abstinence phases. Cognitive decline impairs the response to addiction treatment and increases dropout rates. It can be irreversible, even after the end of drug abuse consumption. Improving our understanding of the molecular and cellular alterations associated with cognitive decline is essential to developing specific therapeutic strategies for its treatment.
Ref: Cognitive Alterations in Addictive Disorders – biomedicines-11-01796
Mental health disorders and substance use disorders (SUDs) frequently occur together (concurrent or dual diagnosis). People may use substances to self-medicate symptoms (e.g., anxiety, insomnia). Treating one without the other often leads to failure in treating both.
First Episode Psychosis programs treat both conditions simultaneously (behavioral therapy, medication management). Focus on building skills: therapies like CBT help develop coping skills for both conditions.
It’s crucial to be honest with healthcare providers about all substances used (including alcohol and cannabis) to prevent severe, harmful interactions. Psychiatric medications work to influence mood and thoughts by balancing chemicals in the brain. Like all medications, there is potential for interactions with foods, prescribed medications, and over the counter medications. This can reduce or cancel the benefits of the medication, including long acting injections.
Mixing psychiatric medication with substances like alcohol, cannabis, or stimulants can dangerously worsen mental health symptoms (depression, anxiety), cause severe physical effects (serotonin syndrome, high blood pressure, breathing issues), reduce medication effectiveness, and increase toxicity, creating a complex cycle where one condition worsens the other, often requiring integrated treatment for both co-occurring disorders.
Key Dangers & Interactions: Alcohol: Amplifies sedative effects (drowsiness, poor coordination), worsens depression/anxiety, and can dangerously slow breathing (with benzodiazepines/opioids).
Stimulants (Cocaine, Meth): High risk of dangerous blood pressure spikes, bleeding (with SSRIs), or Serotonin Syndrome (with MDMA/SSRIs).
Marijuana: Can worsen anxiety/depression, especially long-term, and increase side effects with SSRIs.
Ecstasy (MDMA): High risk of Serotonin Syndrome with SSRIs; can increase movement disorders with antipsychotics.
Opioids/Benzodiazepines: Combined use, especially with alcohol, can cause fatal respiratory depression.
Regional Concurrent Disorders Programs:
CAMH Toronto – Concurrent Disorders Program
St.Joseph Healthcare Hamilton – Concurrent Disorders Program